Today's post will be an update on me, followed by a short review of an article published in 2011 that I recently found online, and then the always exciting monthly blog stats.
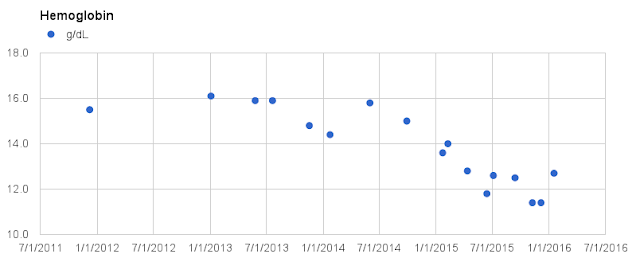
As you may recall from the previous post, at my last physical exam my doctor confirmed I am slightly anemic, and no sources of bleeding were found during an endoscopy and colonoscopy in February. Since then I have had some more blood work done per orders from the gastroenterologist, and I have viewed those results online but have not met with the doctor about them. In my uneducated opinion it looks like I do have iron deficiency anemia. Although all of the numbers related to red blood cells improved slightly from where they were in January, the only one that moved from out of range to within range was hematocrit. Hemoglobin was still low at 12.6 g/dL. Some new numbers from this round of testing were also out of range, specifically ferritin, which was 6 ng/mL (normal range is 20 to 380), and total iron, which was 26 mcg/dL (normal range is 50 to 180).
I also did a more thorough review of the journal articles I have related to fibrinogen amyloidosis, looking not only for mentions of anemia but also spleen. Several articles mention involvement of the spleen in more advanced cases of AFib, possibly causing anemia that is resistant to treatment. Most of the AFib cases mentioned in the articles either do not mention anemia or hemoglobin as part of the patient's initial presentation, or they say the patient's hemoglobin was normal. But I did find two cases where the patients did have anemia when they initially presented with kidney issues.
So it is not unheard of for an AFib patient to have anemia early in the progression of the disease. Maybe I am so special I developed anemia before developing kidney issues. Of course this is all speculation at this point. But I very clearly remember a comment Dr. Benson made during one of the familial amyloidosis meetings in Chicago, when he was discussing the typical progression of symptoms of the various types of familial amyloidosis. He said sometimes you see a patient who hasn't read the book, and their symptoms are not consistent with the typical pattern.
Moving on to the article review, this article appeared in the "Make Your Diagnosis" section of the journal "Kidney International" in 2011.
Title: The Case: Proteinuria in a patient with diabetes (1)
Authors: Srikanth Kunaparaju, Chidi Okafor, Helen Cathro, Vijay Bhola, F. Jackson Ballenger and Mitchell H. Rosnerl (Virginia, USA)
Journal: Kidney International (April 2011)
Here is a link to the PDF file if you would like to follow along: http://www.kidney-international.org/article/S0085-2538(15)54882-5/pdf
Abstract:
A 49-year-old Caucasian man with type 2 diabetes, hypertension, hyperlipidemia and obesity, and no known renal disease presented with 2 weeks of headache and visual disturbances, and a 6-month history of frothy urine. Diabetes had been diagnosed 3 years previously and had been under excellent control; the most recent Hgb A1c was 7.1%. There was no history of end-organ involvement secondary to diabetes, including retinopathy and neuropathy. Serum and urine protein electrophoresis with immunofixation demonstrated no monoclonal proteins.
The abstract is essentially the first paragraph of the article. The only additional information in the first paragraph is that there was no family history of kidney disease. Additional testing found that this patient's serum creatinine was 4.55 mg/dL, which was significantly higher than his creatinine level of 1.22 the previous year. A 24-hour urinalysis study also showed 10.0 grams of protein. A renal ultrasound showed the kidneys were of normal size, so a biopsy was done.
The kidney biopsy was very similar to other fibrinogen amyloidosis biopsies. It was Congo Red positive and it showed obliteration of all glomeruli with very little amyloid elsewhere. The antibody-specific staining intensity was not strong enough for a definitive diagnosis of fibrinogen amyloidosis, so the biopsy tissue was submitted for mass spec analysis. That analysis showed fibrinogen, and genetic testing confirmed the Glu526Val mutation.
The article then gives some basic information about fibrinogen amyloidosis, which there is no need to repeat here. It also states that since fibrinogen is synthesized exclusively in the liver, a liver or liver-kidney transplant is required for long-term success. Near the end of the article there is one sentence that summarizes the purpose for this article. "The rapid progression of renal disease, high levels of new-onset proteinuria, and well-controlled diabetes should suggest a diagnosis other than diabetic nephropathy." In other words, although diabetes is often the cause of kidney disease, nephrologists should not always assume that is the case without looking a little further. If the renal disease progresses rapidly, the patient develops proteinuria, and the diabetes is well-controlled, there may be an underlying cause of the kidney disease that should be investigated.
Next up will likely be a review of a very recent, very special article.
=====Monthly Blog Status Update=====
As of February 29, 2016:
Total posts: 164 (1 in February)
Total pageviews: 37,600 (~800 in January)
Email subscribers: 14 (unchanged)
Total number of countries that have viewed the blog: 110
One new country viewed the blog in February:
Madagascar
=====
Citation:
(1) Kunaparaju S, Okafor C, Cathro H, Bhola V, Ballenger FJ, Rosner MH. The Case: Proteinuria in a patient with diabetes. Kidney International.79(7):793-794.
Edit 4-1-16: Corrected Total pageviews in Monthly Blog Status Update